What are the Stages of Periodontal Disease?
Periodontal disease (gum disease) is one of the leading causes of tooth loss in Los Angeles. Fortunately, recognizing the signs of and treating periodontal disease quickly can help prevent bone loss and permanent damage to your smile.
Understanding the early stages of gum disease—such as swollen gums or bleeding while flossing—can give you an advantage in treating this common oral disease.
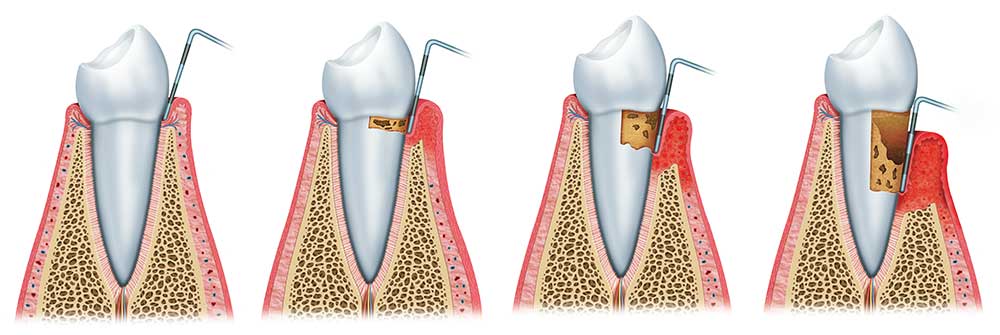
Periodontal Pockets
Before we explain the different stages of gum disease, it’s important to understand how the connective tissue around each tooth attaches to it—specifically, periodontal pockets.
A periodontal pocket is a space that’s created around the root of the tooth when the gums detach, and bone resorbs (due to infection.) Left untreated, pockets will continue to deepen and compromise the stability of the tooth. The depth of each pocket is a major determining factor when diagnosing the stages of periodontal disease.
Here are the various periodontal disease stages and what to look for.
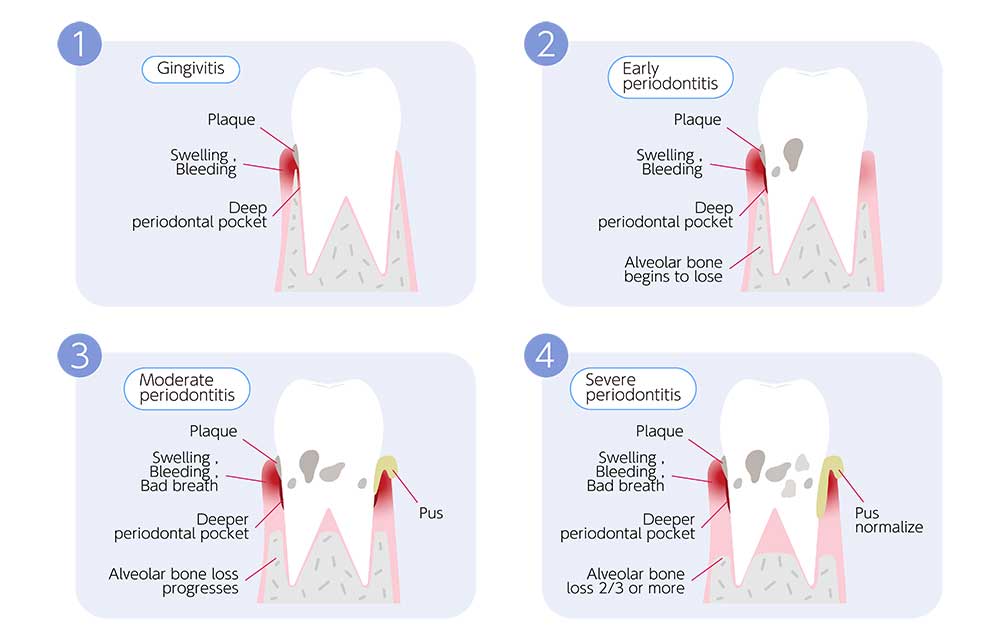
Gingivitis
With gingivitis, there are no periodontal pockets, as the supporting tissues are still attached and stable. However, a collection of dental plaque or tartar left behind from poor oral hygiene habits will trigger your body’s natural immune system to kick in. In turn, the edges of the gums become red, puffy, and bleed easily when you brush and floss.
Gingivitis is the initial stage of gum disease. Treated early, it is completely reversible. But left untreated, the infection will spread deeper into the jaw, causing irreversible damage.

Early Periodontal Disease (Stage I)
Mild periodontitis is the early onset of slight periodontal disease. What makes periodontal disease different from gingivitis is that at this point, bacteria have invaded the gum line and triggered detachment of the tissues. Although the periodontal pockets may be up to 4mm deep, the prognosis is still relatively good.
If you’re not careful, you can easily progress from gingivitis to early periodontal disease without even realizing it, especially if you do not floss each day or see your dentist for preventative care every six months. Many of the typical symptoms of redness and gum inflammation are nearly identical to gingivitis. The only way to know whether or not pockets are beginning to develop is to have a screening completed with your dental provider.
Moderate Periodontal Disease (Stage II)
Moderate periodontal disease is more aggressive than Stage I infections. Pockets are usually up to 5mm deep with slightly visible bone loss on your dental X-rays. At this point, issues such as bad breath or gum recession may also be noticeable. Stage II periodontal disease treatment typically involves scaling and root planing, followed by routine periodontal maintenance.
Advanced Periodontal Disease (Stage III)
Severe periodontitis involves pockets 6mm or greater and the loss of up to four teeth. Vertical bone loss may also be visible on your X-rays. At this point in the disease process, seeing a periodontal specialist is essential. Deep cleanings and periodontal surgery are usually recommended. The prognosis is fair, assuming the infection is caught quickly enough.
Stage IV Periodontitis
Stage IV advanced periodontal disease involves extremely deep periodontal pockets as well as significant bone loss around the roots of the teeth. People with stage IV gum disease usually have several missing teeth and are at risk of losing several more. Usually, this stage requires periodontal surgery and/or augmentation of soft tissues or bone to facilitate smile reconstruction.
But What About Peri-implantitis?
Peri-implantitis is the implant form of periodontal disease. Although dental implants do not develop cavities, the bone and gum tissue around them can still develop advanced periodontitis, especially if home care is not as effective as it should be. Any gum disease around an implant could cause the restoration to fail. Scheduling regular checkups and healthy gum screenings—along with daily brushing and flossing—can help your dental implants last for life. The goal is to prevent any plaque buildup or gingivitis from developing around each of your implant restorations. If you have had poor oral hygiene habits in the past, now is the best time to change them.
Why Does Periodontal Disease Get Worse?
Untreated periodontal disease typically compounds into more aggressive stages of infection over time. Since most of the bacteria lurk below the gumline, pocketing and bone loss can be difficult to assess on your own. The buildup simply continues harboring more bacterial colonies, allowing the infection to spread deeper around the roots of teeth. In time, supporting bone gradually shrinks back as the gum tissues become necrotic and detach from each tooth.

What to Expect During a Periodontal Evaluation
During your initial and recurring periodontal evaluations, our Los Angeles periodontist will thoroughly assess your gum and bone levels, plaque buildup, screen for tartar, and measure the depth of each gum “pocket”. Regular cleanings and exams allow us to pinpoint areas where gum infections are developing or worsening. Although the changes are quite small, they are significant when it comes to something as important as your smile.
Treating Periodontal Disease
At The Center for Advanced Periodontal and Implant Therapy, we offer a wide variety of gum treatments to help preserve your smile (and prevent further infection.) From traditional deep cleanings, osseous pocket reduction surgery and periodontal surgery, non-surgical gum therapy, and advanced non-surgical periodontal therapy like the Bonner Method which can cure gum disease.
Please note we always start with the minimally invasive non-surgical therapy to treat our patients, and we will always do our best in order to avoid any kind of surgical intervention in the future. We begin by doing a very deep cleaning non-surgically, and then reevaluate our patients in four to six weeks to see if there’s any further intervention necessary. If there’s further intervention necessary we will discuss it, and then provide you with minimally invasive options that are comfortable and offer speedy recovery.
We incorporate the best resources for the unique needs of each patient. Ideally, we want to address stages of periodontal infections as early as possible before significant changes in your jaw bone occur.
In some cases, it’s also possible to treat your gum infection so that supporting bone is healthy enough for dental implant placement.
Your oral health isn’t the only thing at stake. Deep bacteria-filled pockets can significantly strain your overall immune system. The more aggressive your gum disease is, the greater the chances your overall health will be affected. The great news is that by treating your periodontal infection, you can enjoy a boost in overall wellness within just a few months.
Reserve an Exam Today
Do you have puffy, bleeding gums or chronic bad breath? Contact The Center for Advanced Periodontal and Implant Therapy in Los Angeles to request an appointment.
You May Also Like...
Senior Periodontal Care and the Challenges Aging Presents
As we journey through the stages of life, there's one aspect that demands consistent consideration — our oral health....
Stem Cells Tissue Regeneration: An Alternative to Classic Gum Graft
Gum recession is a common dental problem that affects millions of people worldwide. This condition occurs when the...
Revolutionizing Gum Disease Treatment: A Non-Surgical Approach to Healing at the Microscopic Level
Gum disease is a widespread oral health issue that affects millions of people around the world. Left untreated can...



